Vertebral metastasis is a common finding in tumors of the prostate, breast, lung and multiple myeloma.
Vertebral metastasis is a common finding in tumors of the prostate, breast, lung and multiple myeloma. Lytic vertebral lesions and vertebrae fractures can lead to severe pain and in due course of time can result in fracture with anterior wedging of the vertebrae. It is a highly painful condition and is usually treated via conservative means or minimally invasive percutaneous vertebroplasty/ kyphoplasty. Conservative management includes use of braces, medications like NSAIDs, calcium supplements, vitamin D, bisphosphonates/denosumab, gabapentin and steroids. Generally, vertebral fractures heal within a few weeks or months with conservative treatments. A subset of patients continue to have pain and remain unresponsive to conservative therapy or report persistent pain despite percutaneous cement procedures like vertebroplasty.
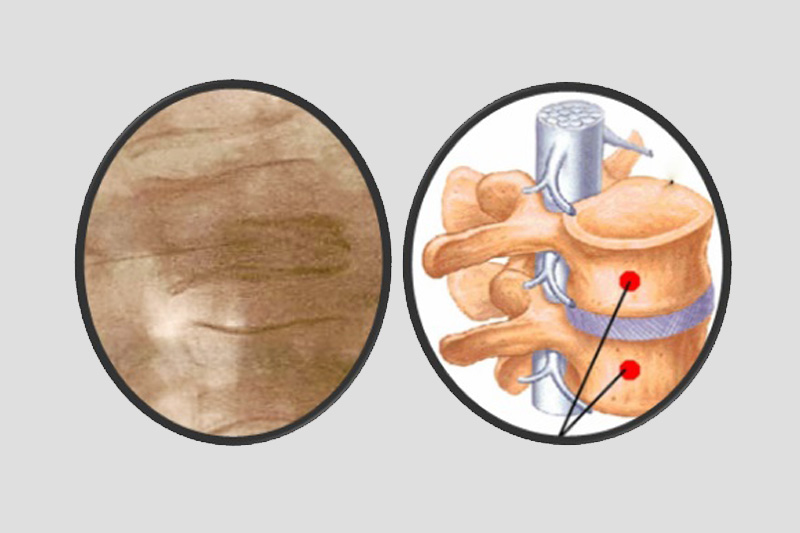
Rami communicans nerve block is a procedure which can be used to relieve persistent severe pain as an adjunct to above mentioned procedures. This nerve block was based on the observation that gray ramus communicans, containing unmyelinated postganglionic fibers rejoin dorsal and ventral rami, distributing around vertebral body wall and course into anterior disc and thus possibly providing major sensory input for vertebral injuries.1
It is performed as a two-stage process and done bilaterally. Once the needle reaches the target point (AP view showing the needles to be hugging the middle to lower one third of the waist of the vertebral body; Lateral view depicting the needle tip in the middle of the vertebral body), final confirmation is done with dye under X-ray guidance. Thereafter, 0.5 to 1.0 ml of local anesthetic with steroid is injected. Radiofrequency ablation can also be done for prolonged effects. Preliminary reports from Oh and Shim suggest that RF thermocoagulation of rami communicans nerves provide significant pain relief as well as an improvement in body function for patients with vertebral body pain.2
To conclude, rami communicans nerve block is a useful and cost-effective adjuvant therapeutic modality in treatment of pain due to vertebral metastatic fractures. With the use of fluoroscopic guidance and expertise, it can be considered a safe option in selected patients where pain persists despite conservative treatment or following vertebroplasty.
Reference :
- 1) Tae HS, Kim SD, Park JY, Kim SH, Lim DJ, Suh JK. Gray ramus communicans nerve block: a useful therapeutic adjuvant for painful osteoporotic vertebral compression fracture. J Korean Neurosurg Soc. 2003;34:505-8.
- 2) Oh WS, Shim JC. A randomized controlled trial of radiofrequency denervation of the ramus communicans nerve for chronic discogenic low back pain. Clin J Pain. 2004;20(1):55-60.